As my husband and I have learned from personal experience, the input we receive from medical professionals along our journey contributes in a huge way to either lightening our burdens or adding to them. The research article I want to highlight today is titled "Our Children Are Not a Diagnosis" (full citation at the end of this post), and the pointers offered to health care providers (HCPs) rang so true when I read them that I felt the information was worth shouting to the world!
First, I want to share some feelings and experiences common to parents who choose to continue pregnancies despite diagnoses of fetal anomalies. Since the research represented input from parents of 107 children with full T13 or T18, I feel we are in good company, with many of the quotes and answers resonating with our personal feelings and experience. Quotes from the article are in italics; I will follow with commentary about our own experience.
Facts:
- "Parents experience intense grief reactions regardless of the choice they make. However, parents who were offered support and who chose to continue pregnancy described a positive experience in all explorative descriptive studies."
- "The majority of parents felt some HCPs did not view children with T13-18 as unique children and that they did not look beyond the grim statistics of these conditions." [This has been true of two of the doctors we have consulted with at various times--but not of the providers I have seen at the military treatment facility.] After diagnosis, parents report being told that:
- Their baby would likely die before or at the time of birth [Check]
- Their baby would not live more than a few months [Check]
- The condition of their baby was lethal or incompatible with life [Insinuated if not in these words]
- Their child would be a vegetable [The actual word spoken to me was "retarded."]
- Their baby would destroy their family or their marriage [Check]
- If their baby survived, he would live a meaningless life or a life of suffering [The word used here was "futile."]
- "The majority (61%) of parents reported feeling pressure to terminate their pregnancy." [I am pleased to say that none of the HCPs I have spoken with either in person or on the phone has even suggested this, but this perhaps may have been different if we had not begun EVERY meeting by firmly telling that particular HCP that abortion is NOT an option for us.]
- When first hearing about the diagnosis, "The most common hope was that the child would be born alive and that parents would have a modest amount of time to spend with their child.... Parents report understanding the implications of the diagnosis and only a few had hopes for a miracle or a cure. These modest hopes reflected acceptance of the serious condition." [This is certainly true for us. I don't want or need HCPs to paint a rosy picture for us. We are well aware of the facts. I DO want them to understand the not-so-negative facts, though.]
Ideally, parents who receive a prenatal diagnosis should also receive the full range of information, including new data about these conditions. The spectrum of outcomes for T13 and T18 babies is extremely wide. With a disproportionately high number of these babies being aborted, the statistics we do have are already skewed. But while the traditional view is to describe these conditions as "lethal" or "incompatible with life," the truth is that when interventions are provided, particularly for those who do not have severe anomalies, the one-year survival rates have been reported to be as high as 56% (in some Japanese studies). And as I learned from the article referenced in my last post, early interventions can make a huge difference in how long a T13 or T18 baby lives after birth. It is true that life spans are still significantly shorter, with a small percentage making it past one year. But why not allow parents the opportunity to make and cherish precious memories no matter how long their child lives?
The article featured in this post concludes with the paragraph below, followed by a list of suggestions to assist HCPs in providing optimal prenatal care. I encourage you to share this post or these suggestions with anyone you know in the medical field; it is obvious that some of the doctors I have seen have not encountered a trisomy 18 pregnancy, and they just aren't sure what to tell me other than parroting the statistics that indicate our daughter will likely die sooner rather than later. In general they are kind, compassionate, and non-judgmental; but neither do they understand that T18 isn't necessarily an IMMEDIATE death sentence. I hope to provide people like them with information that gives a fuller picture of the range of possibilities.
"HCPs need to understand parental perspectives and realize that while T13-18 cannot be 'cured,' the children have value and meaning to their parents regardless of life span and disability. HCPs can provide many positive actions to prepare parents for the life or death of their child. All these interventions result in a measure of 'healing' without cure. Pictures are worth a thousand words. The contrast between family pictures and the pictures of children with trisomy 13 and 18 found in medical texts is striking and demonstrates the contrasting representations of children with these conditions....
Based on the information obtained in this study from parents who continued their pregnancy after a diagnosis of T13-18, we offer suggestions to assist health care providers to provide optimal prenatal care:
- At the time of diagnosis, provide accurate survival figures. Avoid words like "lethal," "incompatible with life," and "vegetable." Avoid value-laden language related to disability.
- Parents should be informed that most parents who choose to continue pregnancy have reported a positive and enriching experience regardless of the lifespan of their child.
- Parents who decide to continue their pregnancy need support, not judgment or pressure to change their choice. Parents accept that early death is likely and they have chosen to value the time they have, both before and after birth.
- Remember that to these parents, their child is a person, not a diagnosis. Refer to the unborn child by name, if possible. Parents expect to receive medical information related to their child, not to the diagnosis. Informing parents of normal organs in addition to anomalies is greatly appreciated. Offer hope when it is reasonable: hope that baby will continue to grow in utero, hope that baby will be born alive and that parents will enjoy some time with the baby.
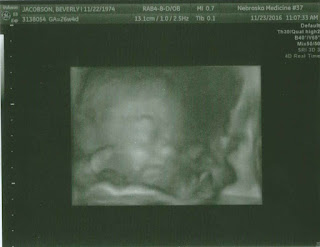
- Offer to continue prenatal and fetal care as for any pregnancy. Ultrasounds are very special, memorable events and given the high risk of miscarriage, might be the only time parents will see their living baby. Taking a few minutes during the ultrasound to point out normal or "cute" features of the baby can be a lifetime gift to parents.
- Guide parents to create a birth plan that is best for their child and family. Parents should understand that children with T13 or 18 are unique and some might benefit from life-sustaining interventions while some may be harmed by them. Ensure that the birth plan includes collectibles for memories such as footprints and photographs. In indicated, be transparent with parents about any hospital protocol or policy that restricts certain interventions to babies born with T13-18. Parental challenges to these restrictions should be discussed in a multi-disciplinary meeting or ethics consultation.
- Most parents who choose to continue pregnancy do so because it is the better path according to their personal beliefs. They appreciate empathy and kindness on their extraordinarily difficult journey, especially recognition of and respect for their love for their child."
*************
NOTE: This post refers to and quotes the following article, noted in italic text throughout the post:
Guon J, Wilfond BS, Farlow B, Brazg T, Janvier A, 2013. Our children are not a diagnosis: The experience of parents who continue their pregnancy after a prenatal diagnosis of trisomy 13 or 18. Am J Med Genet Part A 9999:1-11.
I love that you pour out your heart. As hard as documenting your journey has been, I'm proud of you both. Somewhere out there, your story will help someone else struggling.
ReplyDeleteMellisa Blackburn
That is my heartfelt prayer.
DeleteThis is so good, Beverly. Thank you for sharing all that you are learning on this journey. Your family is not only a blessing to Verity, but to those who will have to walk this path after you. Love you!
ReplyDeleteNice read...very well written
ReplyDelete